
 Revenue Cycle Management
Revenue Cycle Management7 Effective Healthcare Claims Denial Management Strategies

Content
Healthcare denials pose significant challenges, impacting patient care, revenue streams, and operational efficiency. Causes include incomplete patient information, coding errors, and insufficient documentation. Denied claims lead to financial losses, increased administrative burden, and potential patient dissatisfaction.
Most healthcare organizations lose 6 to 8 percent of their total revenue due to payment denials. Healthcare providers cannot ignore a loss of this magnitude, as these payment denials directly impact revenue sources. Managing payment denials well is the key to improving your revenue and winning over your customer's loyalty. An esteemed advisory board states that 90 percent of all claim denials are easily preventable. However, they still occur frequently.
This blog will explain the top 7 strategies to minimize healthcare claims denials.
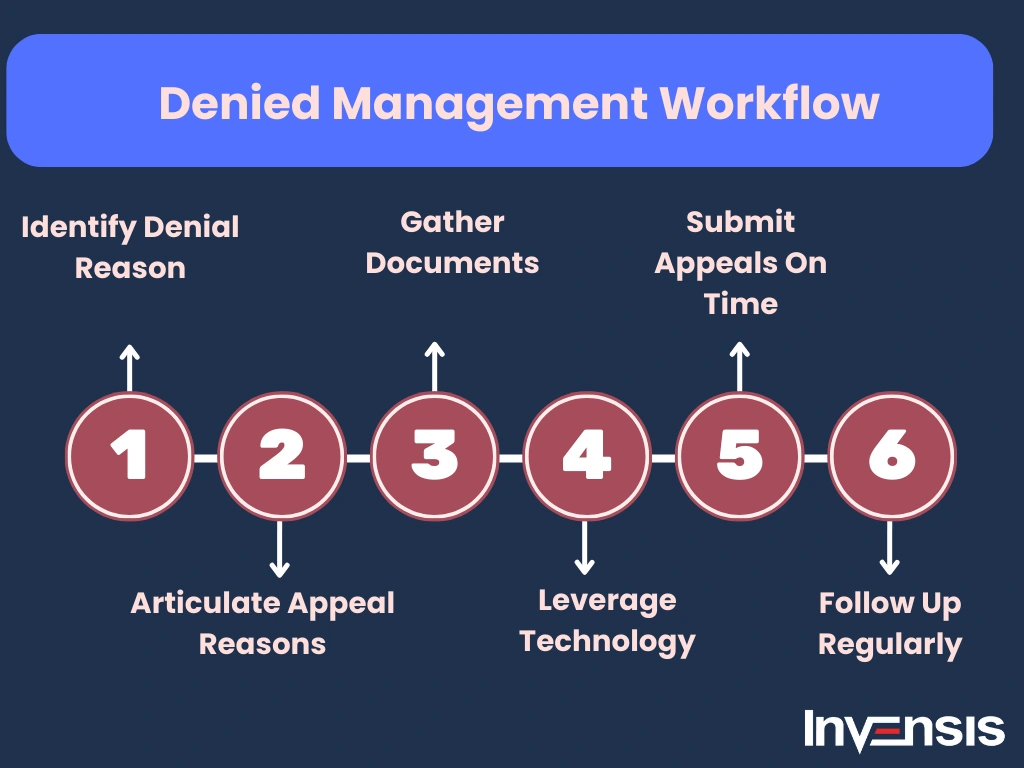
Denial Management - A Detailed Workflow
The denial management workflow typically follows these key steps:
- Identify Denials: Monitor incoming claim denials from insurance providers through explanation of benefits (EOBs) or electronic remittance advice (ERA) systems. Categorize denials by type, such as coding errors, missing information, or medical necessity.
- Analyze Denials: Use denial management software or manual review to determine the root cause of each denial. Common reasons include incorrect patient details, coding discrepancies, authorization issues, or eligibility errors.
- Prioritize Denials: Focus on high-value claims or those with higher chances of reversal. Rank denials based on payer requirements and financial impact.
- Appeals Preparation: Collect necessary documentation, such as medical records, corrected claims, or physician notes. Prepare a strong appeal letter addressing the payer's reason for denial and substantiating the claim.
- Submit Appeals: Send the appeal package to the payer within the specified timeframe. Ensure compliance with payer-specific guidelines for appeal submissions.
- Follow-Up: Track appeal progress and communicate with payers for updates. Use automated systems for reminders and deadlines.
- Resolution and Reporting: Once resolved, update records and analyze trends in denials. Generate reports to identify recurring issues and implement preventive measures.
- Continuous Improvement: Provide feedback to billing, coding, and front-office teams to reduce future denials through training and process optimization.

Fundamentals of Denial Management in Healthcare
Here are some fundamental aspects of medical billing denial management:
1. Understanding Denials:
- Claim Denials: Denials occur when a payer refuses to reimburse a healthcare claim. Denials can be categorized as either hard denials (claims that are not payable) or soft denials (claims that can be corrected and resubmitted).
- Common Denial Reasons: Denials may result from coding errors, incomplete or inaccurate documentation, eligibility issues, lack of pre-authorization, and other factors.
2. Denial Prevention:
- Pre-Claim Checks: Implement processes to perform thorough pre-claim checks to ensure accurate coding, proper documentation, and eligibility verification before submitting claims.
- Training and Education: Regularly train and educate staff on coding guidelines, payer requirements, and changes in healthcare regulations to minimize errors.
3. Denial Identification:
- Monitoring and Reporting: Establish a robust monitoring system to track denials and generate reports. Analyze denial trends to identify common reasons and areas for improvement.
- Technology Utilization: Leverage technology such as revenue cycle management (RCM) software to automate the denial identification process.
4. Denial Analysis:
- Root Cause Analysis: Conduct a clean root cause analysis for each denial to determine the underlying reasons. Address the root causes to prevent similar denials in the future.
- Collaboration: Encourage collaboration between billing, coding, and clinical staff to ensure accurate and complete claim submissions.
5. Denial Appeals:
- Timely Appeals: Develop a streamlined process for appealing denied claims within the specified time frames set by payers.
- Documentation: Ensure that appeal documentation is comprehensive, providing all necessary information to support the claim.

Top 7 Denial Management Strategies to Reduce Claims Denials
Some of the effective tips to improve denial management in healthcare are:
1. Understand Why Claims were Denied
Being aware of why your patient's claims were denied is a critical first step. This awareness helps you to create a streamlined process that maximizes your revenue and helps avoid the pitfalls of claim denials. Your patients may not be fully aware of how the denial system works. In such cases, you also need to educate them about the process and why the insurance claim was denied. Helping your patients through the insurance claim process ensures a strong, long-lasting relationship with them. This timely help provided to your patients goes a long way in contributing to your organization's success. So, understand the reasons for claims denial and clarify them to your patients to ensure the smooth functioning of hospital duties.
Tips to understand claims denial:
- Check eligibility: Confirm patient coverage and policy details to ensure claims align with insurance requirements for reimbursement approval.
- Verify coding accuracy: Review procedure and diagnosis codes for errors, ensuring they align with medical documentation to prevent claim denials.
- Documentation completeness: Ensure thorough and accurate medical records support each claim, addressing any missing or incomplete information that may lead to denial.
- Timely submission: Submit claims promptly to avoid delays and potential denials due to exceeding the insurer's time limit for filing.
- Understand policy exclusions: Familiarize yourself with the insurance policy to identify any specific exclusions or limitations that could lead to claim denials.
- Appeal process awareness: Understand the insurer's appeal process, including deadlines and required documentation, to rectify denials and secure reimbursement for valid claims.
2. Streamline the Denial Management Process
Are you manually fixing your faulty claims? We admit it's an effective short-term solution. However, looking at the bigger picture, you might want to consider a streamlined process. An effective procedure helps you reduce such issues in the future and provides a long-term solution. Losing track of denied claims and having incomplete records threaten your revenue and credibility. Using an organized system to track and manage denied claims to relieve your staff's workload. Newer tools available in the market help your team handle and monitor denials efficiently. So, keep an overall perspective in mind when fixing recurring issues.
Strategies to streamline the medical billing denial management process:
- Automate Verification: Implement automated tools for insurance verification to reduce errors and expedite the medical billing denial management process efficiently.
- Centralized Data Access: Create a centralized database for quick access to patient information, streamlining denial resolution with accurate details.
- Enhance Communication: Foster effective communication between billing and clinical staff to address denial issues promptly and collaboratively for resolution.
- Utilize Analytics: Employ data analytics to identify denial patterns, enabling proactive measures to prevent recurring issues and improve overall reimbursement processes.
- Staff Training Programs: Conduct regular training sessions for staff on denial prevention strategies, ensuring a knowledgeable team adept at handling complex reimbursement challenges.
- Implement Clear Documentation: Enhance documentation practices to provide comprehensive and clear records, aiding in faster denial appeals and reducing potential billing discrepancies.
3. Process Claims in a Week
Did you know that 65 percent of denied claims are never filed again?. Having a proactive claims management team is critical to avoid piling these issues. Your staff should be trained to handle claims well and re-submit any appeals (when requested). Creating a robust denial management workflow to address the claims denial processes assists in founding a strong denial strategy. As soon as you receive a denial from an insurance company, your team should spring in action to process the claim within a week. A hands-on claims team ensures you get paid as soon as possible. If there are some common recurring errors, consider improving your claims filing strategy to address those issues. According to Experian Health, 70% of respondents in their survey indicated that claims management has become increasingly critical compared to its pre-pandemic importance.
Effective Ways to Expedite the Claims Process:
- Verify accuracy: Ensure all claim details are accurate and complete, reducing the chance of errors and delays in processing.
- Streamline documentation: Simplify the submission process by requiring only essential documentation, expediting claim review and approval.
- Utilize technology: Leverage automated systems for claim processing, reducing manual intervention and accelerating the overall turnaround time.
- Prompt communication: Establish clear channels for communication with healthcare providers to address queries swiftly, fostering efficiency in the claims process.
- Continuous training: Regularly update staff on industry changes, ensuring they stay informed about evolving regulations, improving accuracy and speed in claims processing.
- Prioritize high-impact tasks: Focus on critical elements first, addressing high-priority claims promptly to meet the one-week processing goal efficiently.
4. Implement a Claims Denial Log
You can maintain all important data using a claims denial log. An electronic version of the log is an even better choice as it ensures access to relevant information across the organization. You can archive conversations and documentation with several insurance providers to analyze and improve your claim denials. In addition to that, you'll also be able to record the service dates, the demanded amount, the distinct claim numbers, and denied medical codes for easy access in the later stages. Implementing a claim log helps you assess past filing mistakes and improvise for a better coding and billing system. Additionally, using electronic payments saves you 1 minute per transaction. So, record your interactions with the insurance providers to process claims well.
Tips to Implement a Claims Denial Log:
- Document Denial Reasons: Clearly record the specific reasons for claims denials to identify patterns and address recurring issues.
- Categorize by Type: Classify denials into categories (coding errors, eligibility issues, etc.) for efficient analysis and resolution strategies.
- Track Trends: Regularly analyze denial patterns to identify common issues and implement proactive measures to prevent similar occurrences.
- Assign Responsibility: Clearly assign responsibilities for claims denial resolution, ensuring accountability and a streamlined process for addressing denials promptly.
- Monitor Timely Responses: Establish a system to track response times to denials, promoting timely resolution and reducing the risk of missed deadlines.
- Continuous Improvement: Use insights from the denial log to implement process improvements, training, and measures to minimize future claims denials.
5. Identify Common Healthcare Claims Denial Trends
Like all industries, the healthcare industry evolves at an exponential rate. Trends in the claims denial sector keep upgrading to keep up with the transforming healthcare industry. Recognizing different common denial types establishes an effective denial management procedure. Analyzing these trends gives you a deeper insight into the major issues plaguing your claims denial management team. Subsequently, your software upgrades addressing these issues save you money consistently. So, upgrade your knowledge of these trends to have a processing edge over your competitors and save a lot of money.
Tips to Stay Updated to Medical Billing Denial Management Trends:
- Subscribe to industry publications: Stay informed by subscribing to healthcare publications, blogs, and newsletters for the latest denial trends and updates.
- Attend conferences and webinars: Participate in healthcare conferences and webinars to gain insights into emerging denial trends and industry best practices.
- Network with peers: Join professional healthcare networks and forums to exchange information and stay updated on medical billing denial management strategies and trends.
- Engage with industry associations: Connect with healthcare associations to access resources, webinars, and reports highlighting current denial trends and regulatory changes.
- Utilize social media: Follow reputable healthcare professionals and reputed organizations on social media platforms for real-time updates on denials management in healthcare trends and industry news.
- Collaborate with vendors: Engage with healthcare software vendors and consultants who specialize in medical billing denial management to access their expertise and stay current on trends.
6. Outsource Your Medical Billing Denial Management Process
Do you desire a dedicated team to process your claim denials? Consider outsourcing your denial management problems to a capable team. If you outsource well, you can save money and effort and still get efficient claims processing. Expert denial management providers train specialized teams to handle all the complications of the insurance system for you. You'll be able to concentrate on your core competency by delegating these tasks to an efficient company. So, save time, effort, and money by outsourcing your major denial management issues to top firms.
Strategies to effectively outsource healthcare denial management:
- Define Clear Objectives: Clearly outline denial management goals to ensure alignment with outsourcing partners for effective collaboration and resolution.
- Select Experienced Partners: Choose outsourcing providers with proven expertise in healthcare medical billing denial management to enhance efficiency and accuracy.
- Implement Robust Communication: Establish seamless communication channels to share insights, updates, and feedback for swift issue resolution and process improvement.
- Leverage Technology Solutions: Integrate advanced technology tools for data analysis and automation to streamline medical billing denial management processes and boost overall productivity.
- Continuous Performance Monitoring: Regularly monitor and evaluate outsourcing partner performance, utilizing key performance indicators to ensure sustained success and identify areas for improvement.
- Compliance Adherence: Confirm that the outsourcing partner strictly adheres to healthcare regulations and compliance standards, minimizing legal and financial risks.
7. Introduce Incentive Programs
The majority of claim filing errors can be fixed by trained and motivated staff. If you're concerned about the rising software costs, consider incentivizing your staff to reduce your denials. Offer your staff bonuses or time-offs to promote healthy competition that leads to fruitful results. You'll notice a significant reduction in denials when you use these tactics. This technique is truly the most cost-effective and efficient solution to your denial management issues. Also, share valuable information about the trends in the denial management process to help them contribute well to your claim filing processes. So, reward your employees when they do good work to bring you good results.
Strategies for incentivizing healthcare staff:
- Performance Bonuses: Reward teams meeting low denial rates with financial incentives to boost motivation and accountability.
- Ongoing Training Rewards: Encourage continuous learning by offering bonuses for staff completing denial prevention training programs.
- Recognition Programs: Implement a recognition system, acknowledging top performers with public praise and awards for claims denial reduction.
- Team Competitions: Foster a collaborative environment by organizing friendly competitions with rewards for the team achieving the highest claims approval rates.
- Quality Metrics Incentives: Link incentives to maintaining high-quality work, emphasizing accurate documentation and thorough claims processing to reduce denials.
- Flexible Work Arrangements: Offer flexibility or additional benefits for teams consistently achieving low claims denial rates to enhance work-life balance
Conclusion
We are sure you know how to handle several healthcare claims denial management issues well now. So, save 6 to 8 percent of your revenue from these issues using our helpful tips. Focus on incentivizing and training your staff to reduce denials and motivate your team. You could also develop a strong and flexible process to deal with such issues competently. So, don't be the team that slacks and doesn't re-submit claims. Lead a proactive and informed team to retain your revenue.
In many cases, managing an in-house team for medical billing denial management can be complex and time-consuming. Delegating the process to an external provider can ease it. Invensis is a prominent denial management services provider that offers tailored solutions to healthcare organizations. We specialize in navigating complex billing challenges, reducing denials, and optimizing revenue cycles. Contact us today to learn how we can help in reducing your claims denials!
Frequently Asked Questions:
Discover Our Full Range of Services
Click HereExplore the Industries We Serve
Click HereBlog Category
Related Articles

Optimize your store in 2026 with the best WooCommerce order management plugins. Automate order tracking, inventory, and customer service for success.
January 21, 2026
|

Find the leading accounting firms in Singapore trusted by businesses for audit, tax, and advisory services.
November 6, 2025
|

Explore the leading accounting firms in South Africa providing expert audit, tax, cloud accounting, and payroll services. Learn about their key features and unique offerings.
February 2, 2026
|
Services We Provide
Industries We Serve





.webp)