
 Revenue Cycle Management
Revenue Cycle ManagementWhat Are ICD-10 Codes in Medical Billing? List of a Few Complex Codes

Content
ICD-10 (International Classification of Diseases, 10th Revision) is a globally recognized system for classifying and coding diseases, disorders, injuries, and other health conditions. It is used by healthcare providers, researchers, coders, and insurance companies to standardize the classification and coding of medical diagnoses and procedures.
ICD-10 codes consist of alphanumeric characters and are organized into chapters and categories. Each code represents a specific condition or disease and provides detailed information about the diagnosis or procedure being documented. The codes are used for various purposes, including medical billing, statistical analysis, and clinical research.
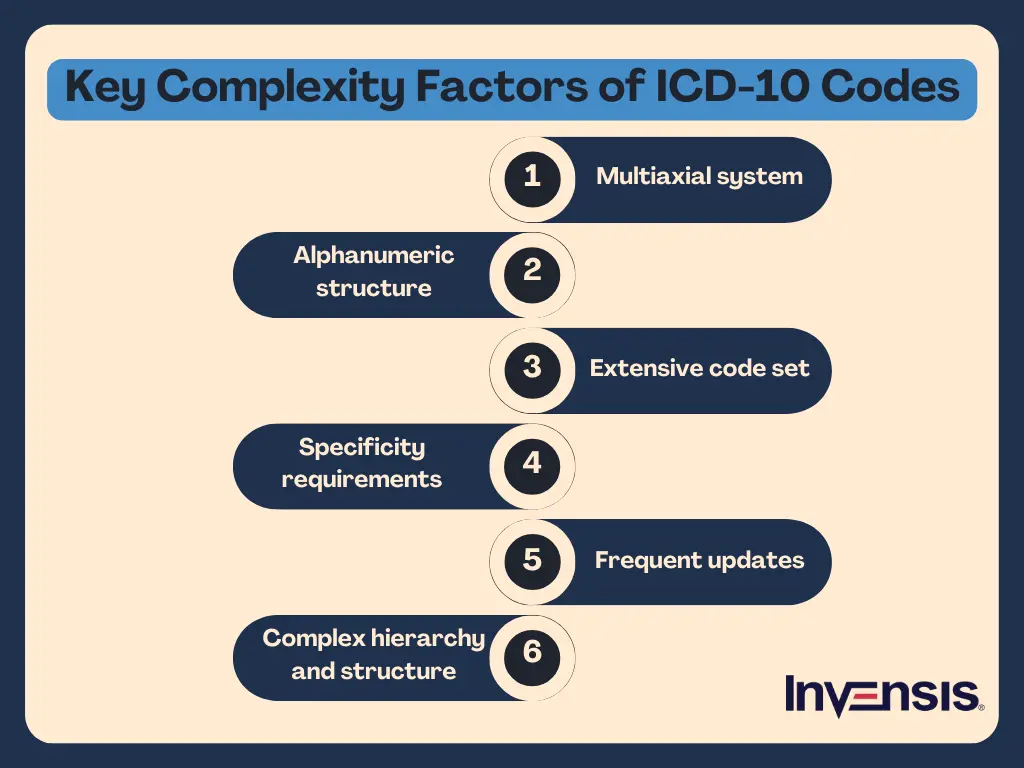
However, ICD-10 codes in medical billing are complex and pose significant challenges for medical billing and coding professionals. Firstly, the comprehensive classification of ICD-10 encompasses a wide range of medical conditions, leading to a large number of codes and increased complexity. Secondly, the granularity and specificity of the codes provide detailed patient diagnosis information, requiring coders to navigate through specific details and increasing the complexity of the coding process. Additionally, the multiaxial structure of ICD-10, with multiple dimensions such as etiology and anatomical site, adds further complexity. Below, we look at a few commonly confused codes
This blog will explain the ICD-10 codes in medical billing and the most complex ICD-10 diagnosis codes listed in medical billing for medical billers and coders.
Most Complex ICD-10 Codes in Medical Billing Records
Here are the ICD-10 codes for easy reference, covering some of the most complex codes for medical coders and billers:
1. ICD-10-CM Diagnosis Code F32.3: Major depressive disorder, single episode, severe with psychotic features
This ICD 10 code for medically complex patients refers to a major depressive disorder, single episode, severe with psychotic features. This code can be challenging to interpret for several reasons:
- Complexity of Diagnosis: Complex mental health conditions with the added challenge of psychotic features indicating hallucinations, delusions, or psychosis.
- Subjectivity of Symptoms: Different patients may express similar symptoms differently or to varying degrees.
- Clinical Judgment Required: Psychotic symptoms can sometimes overlap with other conditions, making accurate diagnosis and coding more difficult.
Healthcare professionals involved in coding must strongly understand mental health disorders and collaborate closely with clinicians to ensure accurate and detailed documentation.
2. ICD-10-CM Diagnosis Code G47.419: Narcolepsy, unspecified
This code refers to narcolepsy, unspecified. This code presents challenges due to the following:
- Varied Symptoms: Narcolepsy includes excessive sleepiness, sleep attacks, cataplexy, sleep paralysis, and hallucinations. Symptoms vary, making classification and diagnosis difficult.
- Differential Diagnosis: Distinguishing narcolepsy from other sleep disorders requires careful evaluation and collaboration between healthcare professionals and clinicians.
- Subjective Nature: Patient descriptions and symptom severity vary, requiring comprehensive and accurate information gathering.
- Multidisciplinary Approach: Collaboration among sleep specialists, neurologists, and psychiatrists is essential for accurate diagnosis and treatment.
Accurate coding of narcolepsy requires an understanding of the disorder and coordination between coding professionals and the healthcare team for precise documentation.
3. ICD-10-CM Diagnosis Code K52.2: Allergic and dietetic gastroenteritis and colitis
The above ICD10 code for allergies refers to allergic and dietetic gastroenteritis and colitis. This code poses challenges due to the following factors:
- Diverse Triggers: Various triggers, such as food allergies, intolerances, and sensitivities, can cause the condition, making diagnosis complex.
- Subjectivity of Symptoms: Symptoms vary among individuals, and reactions to foods or allergens differ, making uniform diagnosis difficult.
- Diagnostic Investigation: Accurate diagnosis involves evaluating medical history, elimination diets, allergy testing, and dietary response, requiring collaboration between healthcare professionals and patients.
- Coexisting Conditions: Allergic and dietetic gastroenteritis and colitis may coexist with other gastrointestinal disorders, requiring differentiation for proper management and coding.
Given these complexities, accurate coding of allergic and dietetic gastroenteritis and colitis requires a thorough understanding of the disorder, comprehensive evaluation of symptoms and triggers, and close collaboration between coding professionals and the healthcare team to ensure precise documentation.
4. ICD-10-CM Diagnosis Code M54.5: Low back pain
Diagnosing low back pain using the ICD-10-CM Diagnosis Code M54.5 presents certain challenges that healthcare professionals and coding specialists must address. Some of these are:
- Broad Spectrum of Symptoms: Low back pain (ICD-10-CM Diagnosis Code M54.5) presents challenges due to its varied symptoms, requiring careful evaluation for accurate diagnosis.
- Differential Diagnosis: Distinguishing low back pain from other conditions demands a multidisciplinary approach involving specialists and precise documentation.
- Subjective Nature of Symptoms: Information gathering is essential, ensuring effective treatment planning and coding coordination.
Accurately coding low back pain (ICD-10-CM Diagnosis Code M54.5) requires addressing the challenges posed by its varied symptoms, differential diagnosis, subjective nature, and the need for a multidisciplinary approach and precise documentation.
5. ICD-10-CM Diagnosis Code N18.9: Chronic kidney disease, unspecified
Diagnosing chronic kidney disease, specifically under the ICD-10-CM Diagnosis Code N18.9, poses certain challenges that healthcare professionals and coding specialists must address. The medically complex patient ICD10 for the above should be addressed by:
- Broad Classification: Code N18.9 encompasses all unspecified forms of chronic kidney disease, challenging specific diagnoses.
- Limited Clinical Information: Lack of detailed clinical data in the code makes it hard to pinpoint the exact condition.
- Overlapping Symptoms: Similar symptoms in various kidney diseases can lead to confusion and hinder accurate interpretation.
ICD-10-CM Diagnosis Code N18.9 remains essential for coding and tracking unspecified chronic kidney disease cases despite its limitations.
6. ICD-10-CM Diagnosis Code R11.2: Nausea with vomiting, unspecified
Diagnosing nausea with vomiting, specifically under the ICD-10-CM Diagnosis Code R11.2, presents certain challenges that healthcare professionals and coding specialists must address. These include:
- Broad Classification: The code R11.2 encompasses all unspecified cases of nausea with vomiting, making it difficult to identify the exact cause and underlying condition.
- Limited Clinical Information: With a lack of detailed specifics in the code, interpreting the precise nature of nausea and vomiting becomes challenging, hindering accurate diagnosis.
- Overlapping Symptoms: Nausea with vomiting can be symptomatic of various underlying issues, leading to ICD confusion and requiring a thorough evaluation to pinpoint the root cause.
Healthcare coders must grasp R11.2's nuances and collaborate with clinicians for precise documentation, enhancing patient care and research.
7. ICD-10-CM Diagnosis Code R51: Headache
Understanding the complexity of the above code is challenging because of the following:
- Broad Classification: Code R51 encompasses various headache types (e.g., tension, migraine), making it less specific for targeted diagnoses.
- Overlapping Symptoms: Different headache types may share similar symptoms, leading to confusion in ICD10 code selection.
- Comorbidity Possibility: Headaches often coexist with other conditions, requiring thorough patient assessment to assign the appropriate code.
Deciphering ICD-10-CM Diagnosis Code R51's complexities requires medical expertise, precise patient evaluation, and differentiated headache types for accurate coding and improved patient care.
8. ICD-10-CM Diagnosis Code Z79.899: Other long-term (current) drug therapy
The above ICD10 code long-term drug therapy is for patients with longer treatment. Despite its clear label, interpreting it can be challenging because it involves:
- Broad Inclusion Criteria: This code covers various medications, leading to ambiguity in determining the specific drug under consideration.
- Lack of Dosage Details: Specific dosages and treatment durations need to be indicated, complicating accurate identification of the therapy.
- Multiple Drug Combinations: Patients may be on multiple long-term medications, making it difficult to attribute the code to a single drug.
To overcome the difficulties in interpreting the ICD-10-CM Diagnosis Code Z79.899, coders and billers must collaborate closely with healthcare providers to ensure accurate documentation of the specific drug therapy and its purpose.
Conclusion
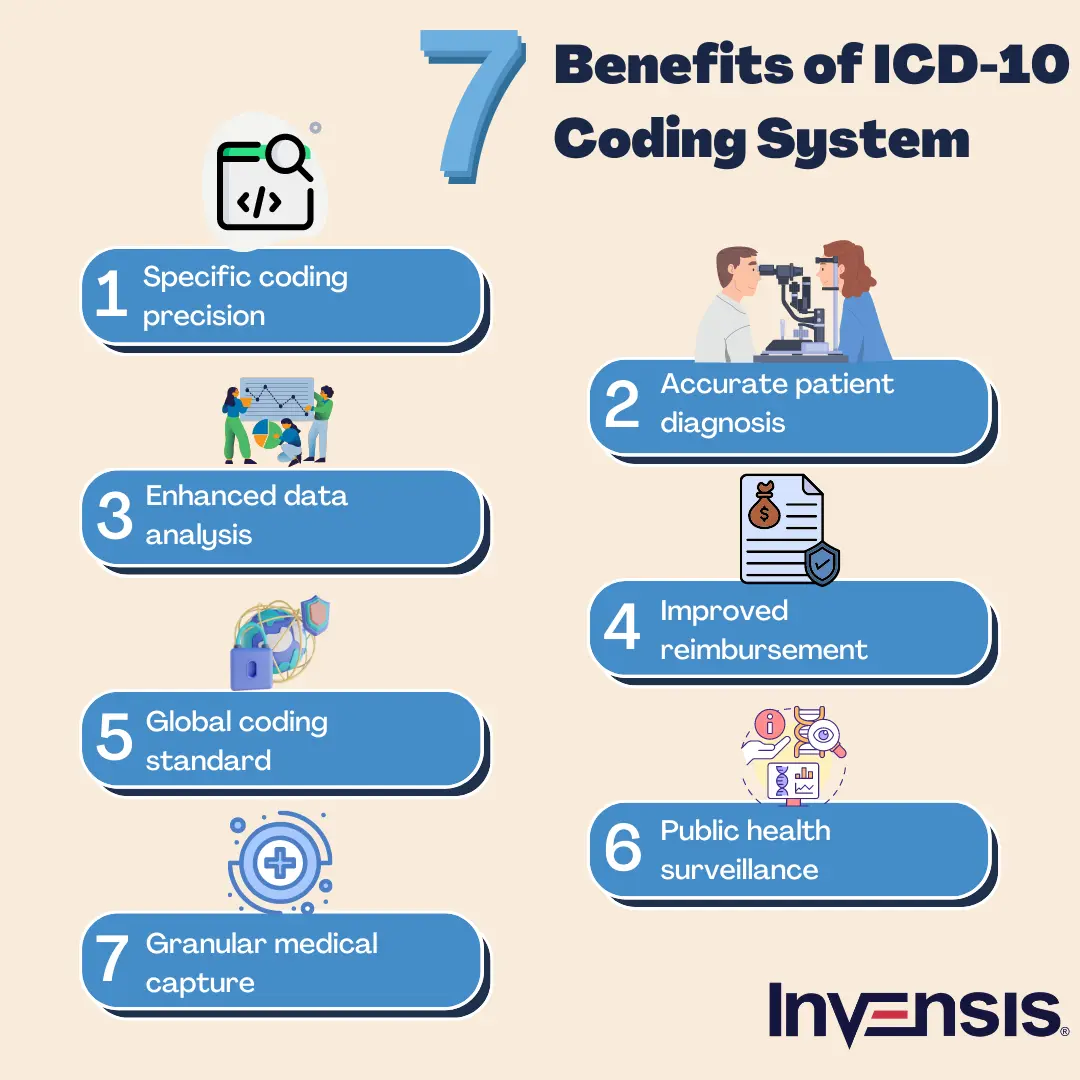
The primary complexities in ICD-10 coding arise from the sheer volume of codes available in the ICD-10 codes in the medical billing system. With over 68,000 diagnostic codes and numerous subcategories, accurately selecting the right code for a particular patient's condition can be daunting. This coding requires meticulous attention to detail and careful analysis of the medical documentation to ensure accurate code assignment. Delegating this task to an experienced medical billing partner will help overcome these intricacies.
Invensis is a renowned medical billing company offering medical billing services to healthcare providers. With our skilled team and extensive knowledge of the ICD-10 codes in the medical billing system, we ensure accurate code assignment, overcoming the complexities of codes. Contact us today to streamline the billing process for maximum efficiency and revenue generation.
Frequently Asked Questions
Discover Our Full Range of Services
Click HereExplore the Industries We Serve
Click HereBlog Category
Related Articles

Find the leading accounting firms in Singapore trusted by businesses for audit, tax, and advisory services.
November 6, 2025
|

Explore the leading accounting firms in South Africa providing expert audit, tax, cloud accounting, and payroll services. Learn about their key features and unique offerings.
November 6, 2025
|

Explore what project accounting is, how it works, and why it’s essential for businesses. Understand key principles, revenue recognition methods, and best practices to improve your knowledge.
October 7, 2025
|
Services We Provide
Industries We Serve





.webp)