
 Revenue Cycle Management
Revenue Cycle ManagementThe Impact of AI on Medical Claims Processing: 9 Key Impacts

Content
Medical claims processing plays a crucial role in healthcare, ensuring that insurers, providers, and patients are accurately reimbursed for medical services. However, this complex process is often plagued by inefficiencies, delays, and human errors, which can lead to frustration and financial losses. As healthcare continues to grow and evolve, the demand for faster, more accurate processing becomes increasingly urgent.
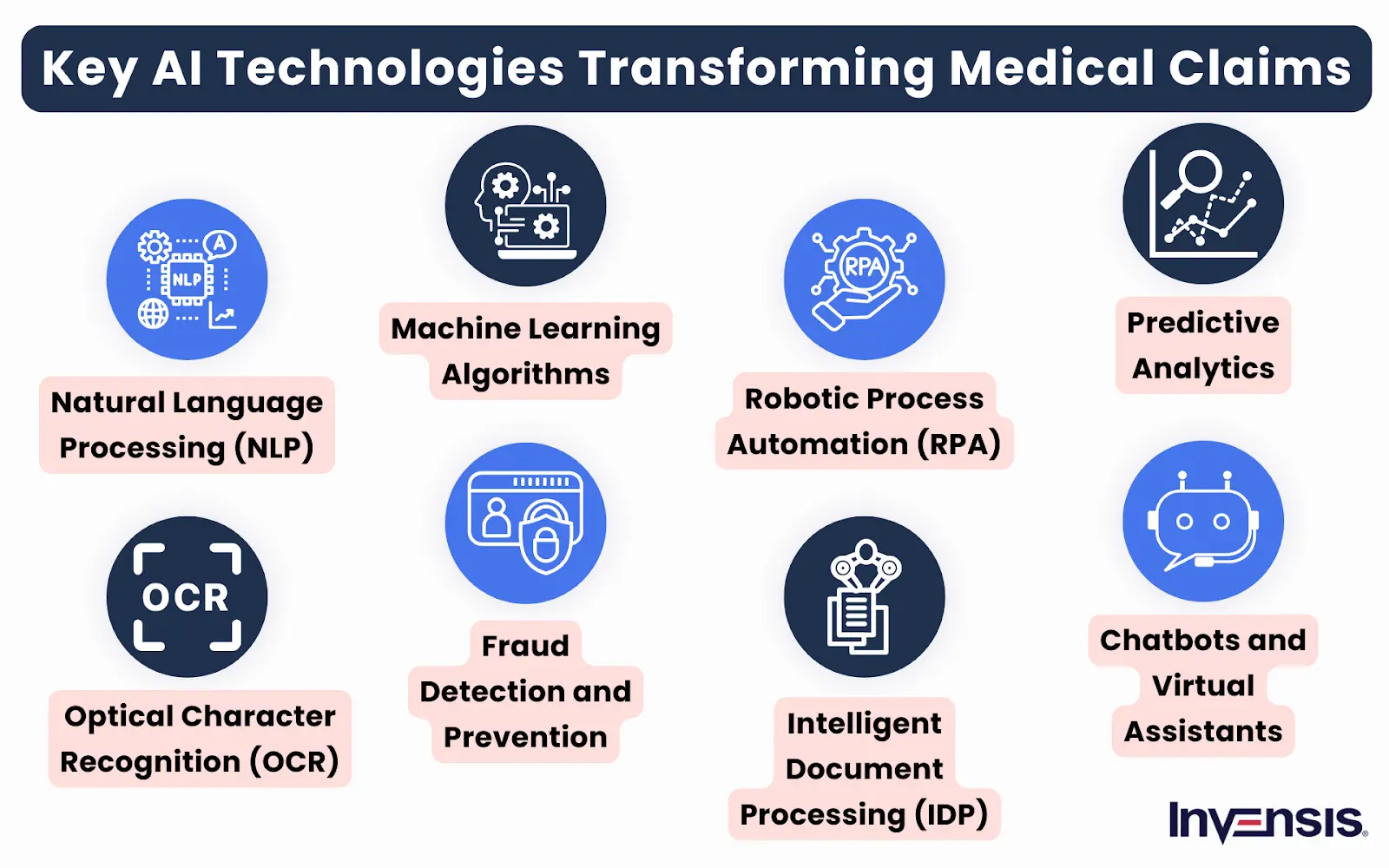
This is where Artificial Intelligence (AI) emerges, offering transformative potential. AI’s ability to automate repetitive tasks, analyze vast amounts of data, and detect patterns quickly makes it a game-changer in medical claims processing. By enhancing accuracy, speeding up workflows, and reducing costs, AI is revolutionizing the way claims are managed.
In this blog, we will explore the top 9 impacts of AI on medical claims processing, demonstrating how its adoption is reshaping the industry and improving overall efficiency.
9 Ways Artificial Intelligence is Redefining Medical Claims Processing
AI is addressing long-standing inefficiencies and challenges in the medical claims management process. Below, we explore the top 9 impacts of AI on medical claims processing operations.
1. Automated Claims Submission
One of the biggest challenges in traditional medical claims processing is the time-consuming, error-prone manual submission process. Healthcare providers and insurance companies often rely on paper-based forms or complex electronic systems, leading to delays, misunderstandings, and increased administrative costs. These inefficiencies cause frustration for both providers and patients, resulting in slower reimbursement and higher operational expenses.
Automated claims submission streamlines the process by using AI and machine learning to automatically capture, verify, and submit claims to insurance companies. AI adoption for claims processing reduces human errors, speeds up claim approvals, and ensures faster reimbursements for healthcare providers.
By automating these tasks, healthcare organizations can free up resources to focus on core patient care and improve overall operational efficiency. AI-powered claims management cuts down processing time and minimizes costly mistakes, improving the accuracy and speed of claims submissions.
2. Enhanced Claims Validation and Verification
A significant challenge in medical claims processing is the high rate of claims being rejected due to inaccuracies or missing information. Manual verification often results in errors that delay the approval process and increase administrative workloads. Providers face challenges in ensuring that all necessary details are correctly submitted, leading to costly rework, disputes, and delayed payments.
AI-driven claims processing enhanced claims validation and verification address these issues by automatically cross-checking claims against pre-established rules, patient data, and insurance policies. This technology identifies discrepancies or incomplete information before submission, reducing the chances of errors or rejections.
By ensuring claims meet all requirements upfront, AI claims automation tools accelerates processing times, reduces administrative costs, and improves the accuracy of claims, leading to fewer delays and a smoother reimbursement process for healthcare providers.
3. Faster Claims Adjudication
Traditional claims adjudication involves complex, manual review processes where claims are evaluated by multiple staff members, leading to significant delays. This often results in a lengthy waiting period for providers and patients, slowing down reimbursements and increasing the administrative burden. The process can also be inconsistent, with human errors leading to mistakes in determining claim validity, further prolonging resolution.
Automation and claims processing algorithms speed up claims adjudication by analyzing large volumes of data quickly and accurately. It is one of the great impacts of AI on medical claims processing. Machine learning algorithms assess claims against relevant guidelines, medical records, and insurer policies, ensuring a faster and more accurate decision-making process.
AI for efficient healthcare claims processing reduces the need for manual intervention and speeds up the approval cycle, ultimately improving cash flow for healthcare providers. AI claims adjudication enhances efficiency, decreases errors, and ensures faster resolution of claims, benefitting both patients and healthcare organizations.
4. Improved Fraud Detection and Prevention
Fraud in medical claims processing is a persistent issue, with fraudulent activities such as upcoding, phantom billing, and duplicate claims causing significant financial losses. Manual systems often struggle to identify these complex fraudulent activities due to the volume of data and intricate patterns involved. As a result, healthcare providers and insurers face substantial financial risks, and patients may experience inflated costs for services.
AI-driven insurance claims management enhances fraud detection by leveraging advanced algorithms to analyze large datasets and detect unusual patterns that suggest fraudulent behavior. Machine learning models can detect inconsistencies, flag suspicious claims in real-time, and prevent fraud before payments are made.
With its ability to continuously learn from new data, AI fraud detection in healthcare improves its accuracy over time, reducing false positives and ensuring that only legitimate claims are processed. Incorporating AI into claims processing helps protect against financial losses but also ensures that resources are directed toward legitimate patient care.

5. Streamlined Appeals Management
Streamlined Appeals Management:
In traditional medical claims processing, the appeals process is often lengthy and cumbersome. When claims are denied, providers must navigate a complicated system to resubmit or contest the decision, which can take weeks or even months. This results in delayed payments, increased administrative costs, and frustration for healthcare providers and patients. The manual process is highly prone to errors, leading to further delays in resolving disputes.
Leveraging AI to improve claims processing streamlines appeals management by automating the review and submission of appeal documents. AI-powered systems can quickly analyze the reason for claim denials, gather necessary information, and suggest corrective actions or alternative solutions.
By speeding up the review process, AI reduces delays and administrative overhead, allowing for faster resolutions. Artificial intelligence in medical insurance enhances the efficiency of appeals and improves the accuracy of resubmissions, ensuring that providers are paid more promptly and reducing the burden on administrative staff.
6. Real-time Claims Status Tracking
Medical claims often move through multiple stages before approval or denial, and keeping track of their status can be a time-consuming process. Healthcare providers are typically left in the dark about the progress of claims, requiring frequent follow-ups with insurers to get updates. This lack of visibility leads to delays, added administrative costs, and uncertainty in managing reimbursements.
AI-powered real-time claims status tracking provides instant, automated updates on the progress of claims. By integrating with both healthcare and insurance systems, AI monitors each claim’s status, alerting stakeholders about any changes or required actions.
This continuous tracking improves transparency, allowing providers to quickly address any issues, manage cash flow more efficiently, and minimize the time spent on administrative follow-ups. With real-time visibility, claims are processed faster, enhancing overall operational efficiency and patient satisfaction.
7. Optimized Resource Allocation
Medical claims processing requires significant administrative resources, with staff dedicating time to tasks like data entry, claim verification, and follow-ups. These manual processes often result in inefficient use of resources, as staff may be bogged down with routine tasks that could be automated. This can limit the capacity of healthcare organizations to focus on higher-value activities and core patient care.
AI in claims management and insurance optimizes resource allocation by automating repetitive and time-consuming tasks, such as data entry, claim validation, and tracking. Medical claims automation tools enable healthcare providers to reallocate their human resources to more strategic activities, like patient care or improving service quality.
AI’s ability to handle these tasks efficiently reduces the need for extensive administrative staff, lowering operational costs. It also enhances decision-making by providing real-time insights, allowing organizations to better distribute their resources where they’re needed most. This leads to increased efficiency and enhanced overall performance.
8. Reduced Errors in Data Entry and Processing
Manual data entry and claims processing are prone to human errors, leading to incorrect claims submissions, rejections, and delays in reimbursements. Simple mistakes such as incorrect patient details, diagnosis codes, or billing information can significantly impact the accuracy of claims and require time-consuming corrections. These errors not only slow down the claims process but also increase administrative costs and cause frustration for both providers and insurers.
Automated claims processing workflow reduces errors in data entry and processing by automating the extraction, validation, and submission of claims data. Through machine learning (ML) and natural language processing (NLP) models, AI can accurately interpret medical records, extract necessary information, and ensure that claims are submitted with minimal human involvement.
Automating the claims management process minimizes the chances of mistakes and ensures that data is processed quickly and correctly. The result is faster claims approvals, fewer rejections, and a more efficient overall process, benefiting both healthcare providers and insurers.
9. Personalized Patient Communication
In medical claims processing, keeping patients informed about the status of their claims can often be impersonal and generic. Patients may not receive timely updates or clear explanations about their claims, leading to confusion, frustration, and reduced satisfaction. This lack of communication can also result in patients feeling disconnected from their care providers, especially when claims are delayed or denied.
AI in healthcare claims processing enhances personalized patient communication by using automated, data-driven systems to send tailored updates regarding claim statuses, approvals, or required actions. Through chatbots, email notifications, and text messages, AI ensures that patients receive relevant and timely information in a way that is easy to understand.
By personalizing communication based on the patient's specific claim and situation, AI increases transparency, reduces anxiety, and improves the overall patient experience. This personalized approach also frees up staff to focus on more complex patient needs while maintaining a high level of service.
Conclusion
The future of AI in medical claims processing holds great promise, with AI enabling faster, more accurate claim evaluations, reducing fraud, and streamlining workflows. However, complexities arise in managing vast data volumes, ensuring regulatory compliance, and dealing with the integration of AI into existing systems. Human oversight is crucial to handling exceptions, resolving disputes, and ensuring ethical decision-making.
To navigate these challenges, many healthcare providers turn to third-party vendors. At Invensis, we deliver medical claims processing services with cutting-edge software designed to streamline claim verification, processing, and adjudication. Our solution automates manual tasks, reducing errors and turnaround times. We offer customized services that include data validation, fraud detection, compliance checks, and reporting.
Reach out to us today to streamline your medical claims processing with our advanced solutions!
Discover Our Full Range of Services
Click HereExplore the Industries We Serve
Click HereBlog Category
Related Articles

Optimize your store in 2026 with the best WooCommerce order management plugins. Automate order tracking, inventory, and customer service for success.
January 21, 2026
|

Find the leading accounting firms in Singapore trusted by businesses for audit, tax, and advisory services.
November 6, 2025
|

Explore the leading accounting firms in South Africa providing expert audit, tax, cloud accounting, and payroll services. Learn about their key features and unique offerings.
February 2, 2026
|
Services We Provide
Industries We Serve





.webp)